Enrolled patients
Enrolment is currently available to residents in Auckland, Bay of Plenty and Canterbury. An enrolled patient is someone who has chosen Tend as their primary care provider.

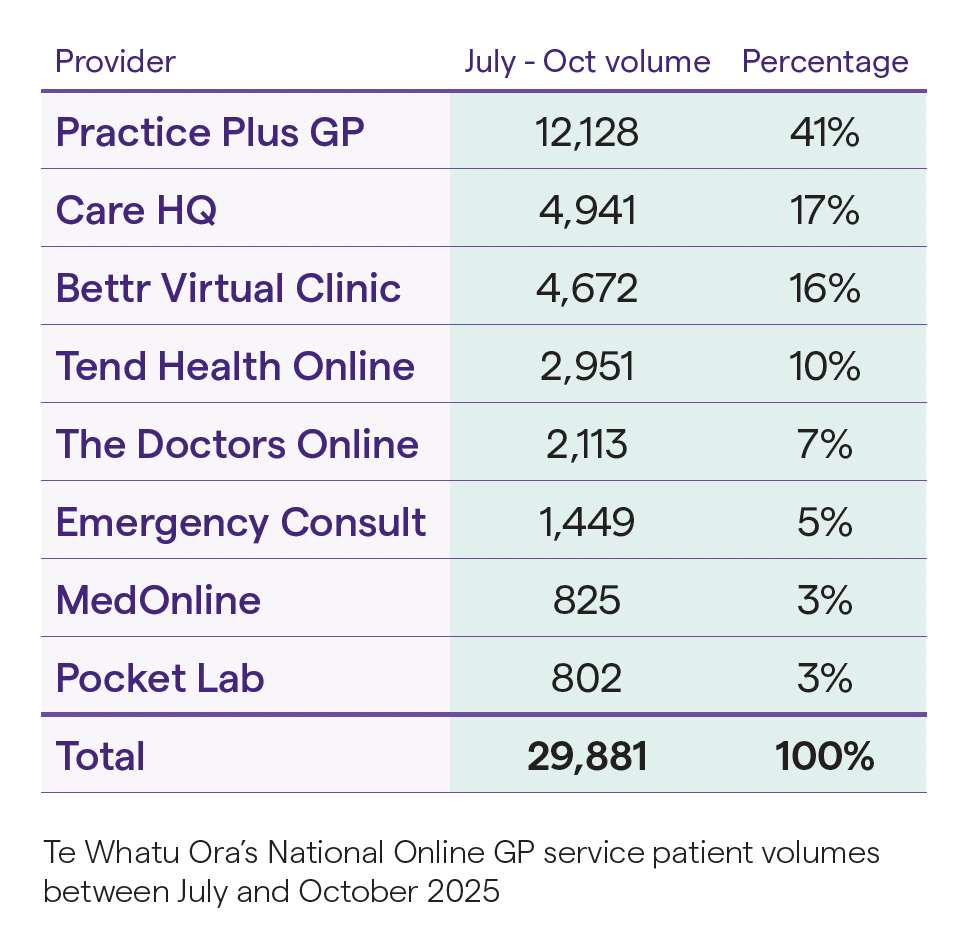
Across Te Whatu Ora’s National Online GP programme more than 29,000 patients were seen between July and October 2025. The largest providers were Practice Plus GP with over 12,000 consultations, followed by CareHQ (~5,000), Bettr Virtual Clinic (~4,700) and Tend Health Online (~3,000). Collectively, this indicates that telehealth is now a significant component of New Zealand’s primary care ecosystem.
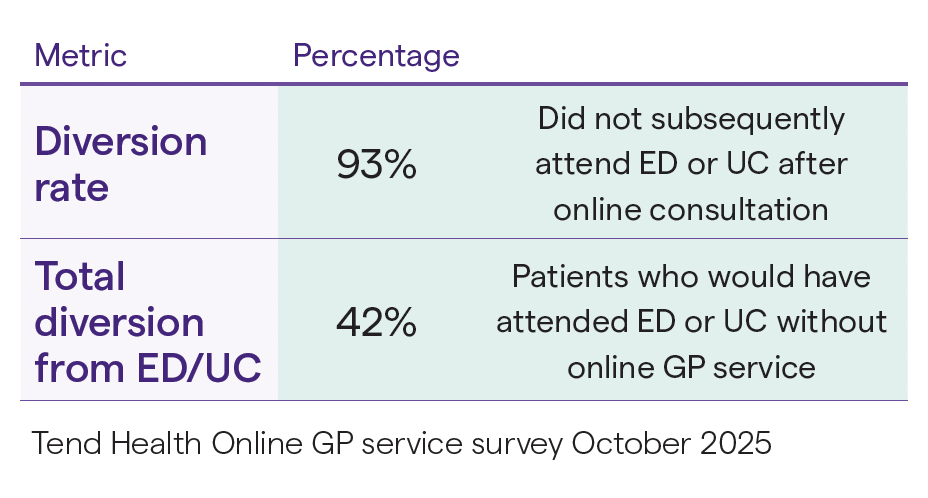
Recent data from Tend Health's service demonstrates significant emergency department diversion alongside workforce capacity expansion. Analysis of 368 patient encounters reveals a 93% successful diversion rate, with 42% of patients indicating they would have presented to ED or UC facilities without online access. Critically, 88% of surveyed clinicians consulting in the service report working additional hours specifically enabled by the online channel, with 44% maintaining workforce participation when they would otherwise have stopped practicing in NZ entirely.
These findings directly respond to concerns from critics who have argued that online GP services are “taking our workforce and making wait times to see a GP worse.” While such concerns reflect legitimate anxiety about resource allocation during a workforce crisis, the emerging data suggests this assumption is unfounded. Conversely, it indicates that online consultations do not simply divert capacity from traditional care, instead improving overall system access and efficiency without compromising clinical quality.
The data: Capacity not competition
Our data reveals clinicians working in online channels at Tend are not redistributing existing capacity but creating new clinical hours that would not otherwise exist. Nearly half report being able to remain in the workforce specifically because online flexibility accommodates circumstances incompatible with traditional practice models. Another 44% state they are working 5-14 additional hours weekly beyond what they are willing or able to commit to in-clinic practice.
The data on the clinical effectiveness of the online service is also compelling. 87% of patients rated their concerns as urgent (19% ‘very urgent’) and of 152 patients who would have sought ED or UC without online access, successful clinical resolution occurred in 93% of cases (with 7% going on to ED or UC assessment).
It is critical that this ED diversion is accompanied by workforce expansion rather than redistribution. While the surveyed numbers are small the data reveals two distinct mechanisms of capacity expansion: those clinicians maintaining workforce participation when they would otherwise have exited, and those prepared to work increased hours in telehealth beyond those they are willing or able to work in-clinic.
This data on Online GP services does not diminish the importance of routine in-person GP care. Rather, the ability to manage appropriate acute presentations through these services will create capacity for face-to-face care where physical examination and continuity of care is needed. This should be viewed as rational resource redistribution, not a decrease in general practice capacity or quality.
System-wide implications
Extrapolating these findings across the thousands of monthly consultations delivered through Te Whatu Ora's national Online GP contract suggests substantial system impact. If 42% of online patients would otherwise present to emergency departments, and 93% are successfully managed without subsequent ED attendance, we observe meaningful decompression of acute services while simultaneously expanding primary care workforce participation.
These outcomes occur during standard practice hours as well as after-hours. While some critics argue that daytime consultations could theoretically be handled by traditional practices, this overlooks the 72% of patients using online services who couldn't secure timely in-person appointments, not through choice, but through genuine access barriers. When these patients face the alternative of emergency department presentation, successful online GP resolution represents system efficiency, not competition.
The path forward requires the sector to move beyond zero-sum thinking about primary care resources. When online channels demonstrably enable GPs to contribute hours they otherwise could or would not, while successfully managing acute presentations that would otherwise burden acute services, they become part of the solution to our capacity crisis rather than a contributor to it.